Safe and Fun-Filled Summer: Kids’ Safety With Dr. Kate Cook
- Category: Educational
- Posted On:

As the Memorial Day weekend approaches and families gear up for summer activities, it's essential to prioritize the safety and well-being of our children. Dr. Kate Cook, a Pediatric Hospitalist at Norman Regional’s Hospital sheds light on crucial aspects of summer safety.
Dr. Cook gives expert advice on several kid-focused topics, including sunscreen and sunburn, water safety, heat exhaustion, dehydration, and the importance of physical activity. Let's dive in and ensure a safe and enjoyable summer for our little ones.

Shielding Kids From Sunburn: The Importance of Sunscreen
Dr. Cook emphasizes the significance of protecting children's delicate skin from harmful ultraviolet (UV) rays and says it’s important to get back in the habit of using sunscreen.
“We usually think about sunscreen when we're going to the pool and have plans to be out in the sun for a long period of time, but we need to think about it on a daily basis,” Dr. Cook says. “It's a good practice to get into applying sunscreen.”
Another option Dr. Cook says to use to protect the skin is UV-protective clothing.
“Some clothes are actually labeled as UV protective. A rule of thumb is just to go for a tightly woven fabric,” Dr. Cook says. “If you hold it up to the light, there shouldn't be much light passing through and that will provide some protection too, especially for kids who can't stand sunscreen.
Risk of Sunburn and Skin Cancer
Applying sunscreen with a sun protection factor (SPF) of 30 or higher is crucial. She recommends generously applying sunscreen to all exposed areas, including the face, neck, arms, and legs.
Then every two hours, or more frequently, reapply if swimming or sweating - this is vital for continuous protection. Without the use of sunscreen or UV protective clothing, the skin is at risk for sunburn.
“Most of your sun exposure happens during childhood,” Dr. Cook says. “Sunburns that happen in childhood do carry a risk for skin cancer down the road. We really want to avoid it as much as possible.”
Dr. Cook says it's pretty universally accepted that mineral-based sunscreens are safe. For example, sunscreen with zinc oxide or titanium dioxide of at least 20%. Those are usually the ones that have the white tint to them, Cook says.
“A lot of times they'll come in a stick, that's handy to use on your face. So those are good to use, and any sunscreen, regardless of the components of it is better than no sunscreen,” Cook says. “It would be best to let the sunscreen soak in for 15 to 20 minutes before you're actually out in the sun.”
Battling the Heat: Heat Stroke and Heat Exhaustion
High temperatures during summer can lead to heat-related illnesses like heatstroke or heat exhaustion, especially in children. Dr. Cook stresses the importance of keeping kids hydrated by encouraging them to drink water regularly.
“One thing to be aware of is we're not used to the high temperatures yet,” Cook says. “Most of the injuries will happen before your body is really acclimated to the hotter weather.”
Dr. Cook urges parents with younger kids to keep an extra eye out for symptoms of heat-related illnesses.
“The things that you're watching for, it's kind of a spectrum of complications from just heat exhaustion, or fatigue, to heat stroke,” Cook says. “The initial symptoms to be watching for would be excessive tiredness, lightheadedness, and feeling like you just can't continue the activity. It's very important to listen to your body and for parents of younger kids to watch their activity level.”
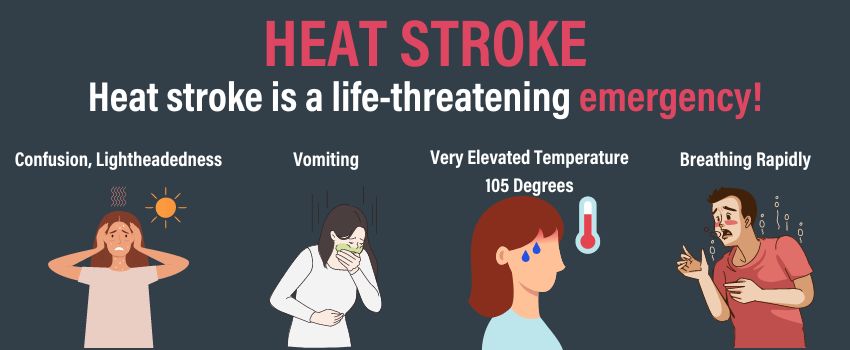
The more serious symptoms to look out for are related to heat stroke.
“More concerning symptoms to watch for that may indicate heat stroke would be a very elevated temperature like 105 degrees,” Cook says. “Confusion, lightheadedness, vomiting, sometimes breathing rapidly or deeper than normal. These would all be emergency signs.”
Heat stroke is a life-threatening emergency that has to be addressed immediately.
Additionally, she recommends planning outdoor activities during cooler times of the day. It’s best for activities outside to be before 11 a.m. or after 3 p.m. to help reduce the risk of UV exposure and also heat exposure. Staying in shaded areas and avoiding prolonged exposure to direct sunlight are also recommended.

Hydrate, Hydrate, Hydrate
It's important that kids have access to water anytime they need it and can take breaks as often as they would like especially in the heat of the day. Dr. Cook says the best thing to keep hydrated is simply water. She says there are certainly electrolyte-rich drinks out there but you need to be cautious of the sugar content.
“Kids don't need drinks with added sugar,” Cook says “Water would be the preferred drink of choice to stay hydrated.”
Babies under six months old should not be getting water, they should be getting breast milk or formula.
“Their bodies just don't regulate their electrolytes well, so it can actually be dangerous to give a baby under six-month-old water,” Dr. Cook says. “Once they get above six months old, a baby could have four to six ounces a day of just strictly water in addition to their breast milk or formula. Then once you're in that age range of one to three, they should be getting about four cups of water a day. Then around age eight, should be around eight cups of water a day.”
Easy signs to look out for include making sure your kid's lips and mouth are wet.
“For babies, when you notice that they're not making tears anymore when they're crying and sometimes young babies, their soft spot on the top of their head, could actually be sunken inward a little when they're dehydrated. Also not having at least three to four wet diapers in a 24-hour period,” Cook says.
Dive Into Water Safety
Water activities can be a refreshing way to beat the summer heat, but parents must be aware of the risks associated with water-related accidents. Dr. Cook advises parents to supervise children closely while they swim and never leave them unattended. A term that some parents might hear around a water scene is “dry drowning.”
“Dry drowning gets a lot of attention because it's terrifying to think about,” Cook says. “It's not really a medical term. But when a child or an adult has had a choking incident where they've gotten some water into their lungs, then later after they're no longer in that water environment, they develop fluid in their lungs from that irritation of what they choked on. That can cause difficulty breathing and exchange of oxygen. It's very rare.”
Dr. Cook encourages parents to be vigilant about coughing or choking in the pool and says dry drowning is rare with the more realistic threat as actual drowning.
It's important to teach children about water safety, encourage the use of life jackets when appropriate, and be vigilant for any signs of distress following a water-related incident.
“Most of the drowning events with kids happen when kids are not supposed to be swimming,” Cook says. Make sure that if you have all access to a pool or lake or body of water, it’s controlled. Meaning, a fence on all sides of a pool that's at least four feet tall with a self-closing self-latching gate, and the kids can't climb over. And remember, that applies to above-ground pools, too.”
While on a body of water like a lake or river, Dr. Cook encourages everyone to wear a lifejacket. In or around a body of water Dr. Cook says you should designate a water watcher.
“An adult around the pool that should be their only job,” Cook says. The adult shouldn’t be on their phone or reading a book or doing anything else. If you have a non-swimming child who is not able to swim independently, they need to be within arm’s reach of an adult at all times.”
Picking the right color of swimwear is also a great way to increase the visibility of children in the water, which typically has a cool tone or blue hue in environments like swimming pools and the ocean.
Avoid swimwear that is blue, navy blue, dark blue and colors within the blue spectrum. Green and purple swimwear can even sometimes blend into the water, depending on the color of the pool liner or tiles. Instead, opt for bright, contrasting colors that will make the child wearing the garments stand out against the blue water backdrop.
Pick out swimwear for your child that is red, orange, pink, bright yellow, and any pattern that won’t blend into the water. This will allow you to keep an even better eye on them, especially if they dip their heads below the surface to dive for toys or swim underwater.
The Power of Play: Importance of Physical Activity
While safety precautions are essential, Dr. Cook reminds parents about the importance of physical activity for children's overall well-being. Engaging in age-appropriate activities promotes healthy growth and development. Encourage outdoor play, bike rides, hikes, and organized sports while ensuring children are adequately protected from sun exposure and heat-related risks.
As we gear up for Memorial Day weekend and the summer season, it's crucial to prioritize the safety and well-being of our children.
Dr. Kate Cook, a Pediatric Hospitalist at Norman Regional’s Hospital, shared valuable insights on topics such as sunscreen and sunburn, water safety, dehydration, and the significance of physical activity.
By following these expert tips, we can ensure that our kids have a safe and enjoyable summer, filled with lasting memories.
Remember to take precautions, be vigilant, and make safety a top priority. Here's to a fantastic summer season for the whole family!
Norman Regional’s Emergency Departments
Norman Regional Health System operates four 24-hour Emergency Departments. Norman Regional Nine, Norman Regional Porter, Norman Regional Hospital, and Norman Regional Moore.
Norman Regional Hospital’s Emergency Department is among the top five busiest in Oklahoma, with 44 beds and more than 70,000 annual visits from patients in and around Norman.
Our average patient length of stay is nationally competitive — currently less than two hours for treated and released patients. We provide comprehensive care delivered by teams of board-certified emergency physicians and trauma and critical care skilled registered nurses, ED techs, secretaries, and lab assistants.
During peak hours, five teams of physicians and staff work to treat patients quickly and safely.



.png)